This disease affects both men and women. Because this disease can cause blindness, early diagnosis and treatment are essential. That is one reason why it is important to have your eyes examined yearly, especially if you are a diabetic or if you have a family history of diabetes.
Diabetic Retinopathy is the leading cause of blindness in the United States.
During a comprehensive eye examination, your optometrist gets to know you, your family, your lifestyle, your primary care provider and your vision needs. The best predictor of diabetic retinopathy is the duration of the disease. For Type 1 diabetic patients, there is no risk of retinopathy for roughly 5 years after initial diagnosis. Some retinopathy is present in up to 50% of patients 10 years after diagnosis. After 15 years, 95% of patients show some retinopathy. The trend for Type 2 diabetic patients is similar. Many Type 2 patients are asymptomatic for years prior to diagnosis and therefore, may present with retinopathy at the same time as being diagnosed for diabetes. Hyperglycemia is a key factor in the development of diabetic retinopathy. Your optometrist will provide communication of diabetic ocular health with your Primary Care Provider and Endocrinologist.
To detect diabetic retinopathy, your optometrist will complete a comprehensive eye examination, including:
- Slit Lamp Evaluation- an examination of the anterior portion of the eye to observe diabetic changes in ocular health
- Dilated Fundus Evaluation- an examination of the back of the eye to observe the health of the retina.
- Optical Coherence Tomography (OCT)- is an imaging technique that uses coherent light to capture micrometer resolution or high-resolution imaging of the retina.
- Retinal Photography- is mainly used to monitor the progression of the diabetic retinopathy
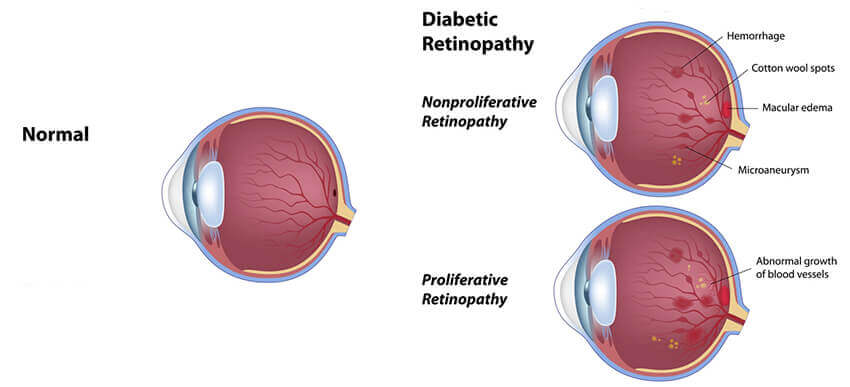
The beginning stages of diabetic retinopathy may cause blurriness in your central or peripheral (side) vision, or it may produce no visual symptoms at all. It mainly depends where the blood vessel changes are taking place in your eye’s retina (the light-sensitive tissue at the back of the eye where images are focused). As diabetic retinopathy progresses, you may notice cloudiness in your vision, blind spots, or floaters. This is usually caused by blood leaking from abnormal new vessels which block light from reaching the retina.
In advanced stages, connective scar tissue forms in association with new blood vessel growth, causing additional distortion or blurriness. Over time, this tissue can shrink and detach the retina.
Once diabetic retinopathy has been diagnosed, your optometrist will determine the degree of diabetic retinopathy. The optometrist will assess a mild, moderate, or severe degree of retinopathy and will schedule regular appointments as necessary to prevent vision loss. The optometrist will work closely with the primary care provider, endocrinologist, and retina specialist to provide preventive care to reduce vision loss or blindness.
Not every diabetic patient develops retinopathy, but the chances do increase after having diabetes for several years. Evidence suggests that maintaining a healthy lifestyle, exercise regularly, diet and avoiding smoking are important risk factors. Taking your medications as prescribed and having your eyes examined regularly are important to enjoying a lifetime of good vision and health.


